Sunspots. Practical advice for skin conditions and skin cancer.
In New Zealand we have one of the highest rates of skin cancer in the world. Caused mainly by over exposure to the sun’s UV rays and also because our clear air and sky means higher levels of UV radiation than in countries with more pollution. As well, the ozone layer is thinner over New Zealand than other countries. The ozone layer blocks UV rays. A sunspot may appear anywhere the skin has been exposed to the sun. Particularly on the hands, scalp, face, back, ears and chest. Sunspots are brown, flat patches that result from melanin. Melanin is a pigment that is produced by cells called melanocytes in response to UV radiation. Melanocytes also cause moles and other pigmented skin lesions. When they become cancerous, they cause melanoma. Another term for sun spots is age spots.

Sunspots can be treated with creams, liquid Nitrogen or intense pulsed light (IPL) to reduce their appearance. We recommend these treatments by a qualified nurse therapist. It is important that your therapist can identify when your spot is a sunspot and not something more serious.

What to do if your sunspot becomes active or bleeds
Sunspots are benign. If they begin to change, it is important to get them checked. Complete our online enquiry for a consultation. Include photos. All to put your mind at ease.
Please check your sunspots regularly
Check your sunspot regularly for any changes in appearance like:
- rapid growth in size
- increased redness
- any tenderness
- ulceration, where a wound forms that won’t heal
- pain or bleeding
- anything else that makes you aware it is different.
It is important to look for these warning signs and any changes in size, shape or colour, the development of irregular borders, itching or if the spot becomes raised or more scaly. There may have been a reason why you suddenly scratched it or caused it to bleed.

Credit: Cancer Society
Changes in your sunspot could indicate signs of progression to skin cancer, such as melanoma or lentigo maligna (a condition that can transform onto invasive melanoma). If you have any questions or doubt, if you have a family history of skin cancers, please get in touch.
What to do if your sunspot is bleeding
If you accidentally catch or scratch your sunspot and it begins to bleed:
- Gently wash the area with mild soap and water to reduce the risk of infection.
- Apply gentle pressure with a clean tissue or sterile gauze for several minutes until the bleeding stops.
- Once the bleeding has stopped, you can use an antiseptic ointment to further protect against infection.
- Place a clean bandage or plaster over the area to keep it protected while it heals.
- Keep an eye on it for signs of infection (increased redness, swelling, warmth, pus or pain).
We recommend sun protection
It’s never too late to become more sun savvy. Along with applying a high-rating SPF sunscreen all year round, we recommend covering up when out in the sun, especially in the hottest parts of the day. Wear sunglasses, a sunhat and reapply sunscreen regularly, even on cloudy days and in winter.
How do I know if my mole needs checking?
Moles are common skin growths that most people have. Most are harmless. If you feel your mole needs checking, get in touch. Early detection of skin cancer, including melanoma from a mole that is changing or becomes symptomatic, is key to a successful diagnosis and treatment.
We also recommend a consultation if your mole is on a place on your body where it rubs on clothing or is otherwise annoying.

These are signs to watch out for if a mole needs checking
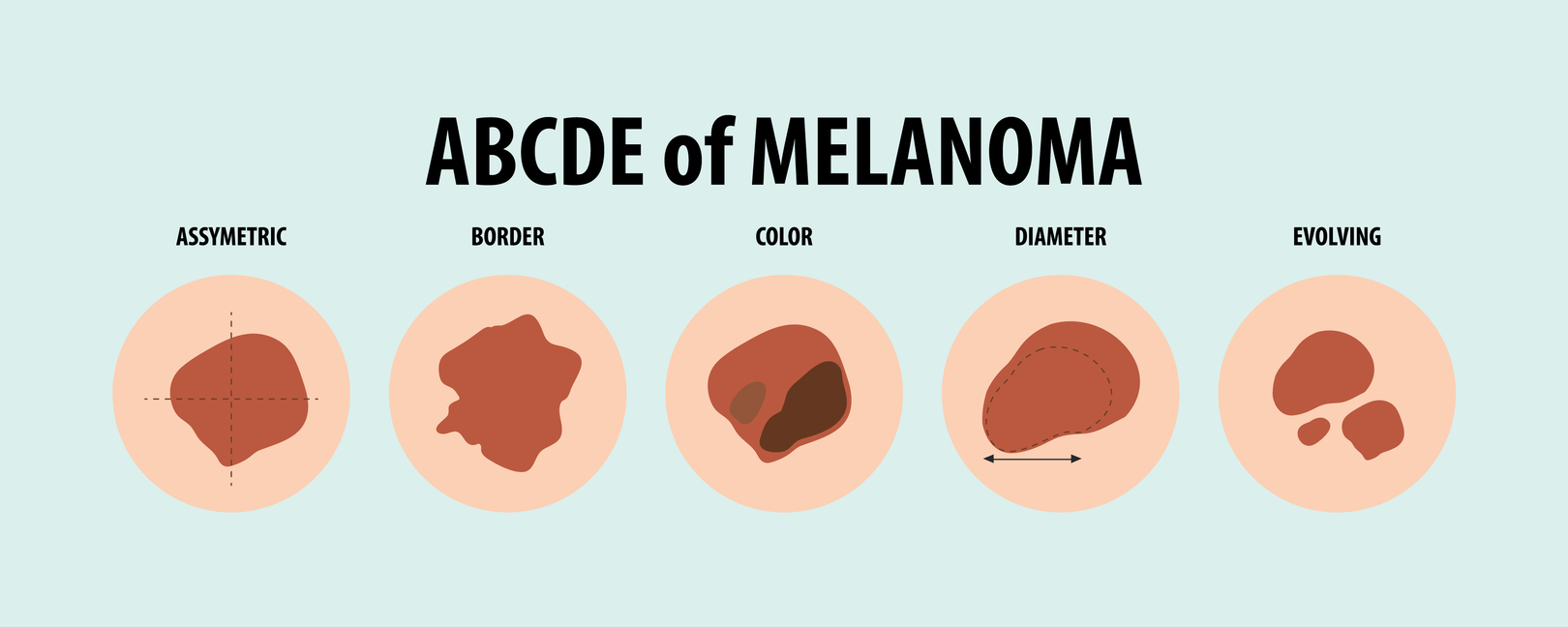
- Asymmetry: One half of the mole does not match the other half in shape or colour.
- Border: The edges of the mole are irregular, ragged, notched or blurred.
- Colour: The mole has uneven colouring with shades of black, brown, tan, red, white or blue.
- Diameter: The mole is larger than 6mm across (about the size of a small pea), though melanomas can be smaller. Or you notice your mole has grown, becomes itchy, bleeds and has changed in shape, size or colour.

We also recommend a consultation if a new mole appears after age 30 and doesn’t disappear again. Let us know if you have a mole that is different to your other moles. Itchy, tender or bleeding moles (if not caused by clothes rubbing) also need to be checked by our team.
Keep an eye on your moles; so you know if one has changed, grown or simply appeared. Take photos with an object in the frame, like a pen. Then compare the photos over time. Get in touch with us to put your mind at rest.
Self-examinations and professional skin checks are recommended if you have risk factors like fair skin, a history of sunburn or a family history of skin cancer.
Will the surgeon remove my mole?
Send us photos (using our 'booking enquiry' form) of the mole you are concerned about. We will get in touch to arrange a consultation. Our surgeon will either remove the mole, and send it off for analysis, or advise that it is doesn't need removing and recommend you keep an eye on it.
Most mole removals can be done under local anaesthetic. You are awake throughout in what is a relatively comfortable procedure. Small, dissolvable stitches will close the wound. Sometimes the surgeon will use stitches that will need to be removed. You can easily organise this at your local medical centre or with one of our specialist nurses. We will give you instructions on how to take care of your wound and how to minimise any scarring. Talk to us today.

New, unsightly or suspicious lumps and bumps? Should you get them checked?
Our skin interacts with our environment, providing a barrier and protection at the same time. Our skin can also signal when something may not be quite right. Sometimes lumps and bumps appear, either within the skin or just beneath it. Here we talk about what to do about a 'new or suspicious' lump.
When should you worry about suspicious lumps and bumps?
A skin lump or bump may appear either slowly or grow reasonably quickly. It can be painless or tender. It may also be unusual in that it is a different colour or texture to your skin. While most lumps and bumps are benign, for example, cysts, lipomas or neurofibromas, some are more serious, including skin cancers, for example, melanoma, basal cell carcinoma (BCC) or squamous cell carcinomas (SCC).

Why suspicious lumps and bumps matter
You should always get new lumps and bumps checked by your general practitioner, nurse practitioner, surgeon, skin specialist or dermatologist, especially it they have some of the characteristics above. As with any medical issue, the sooner you get on to an issue the better the outcome.
Is my lump a melanoma?
More than 7,000 melanomas are diagnosed in New Zealand every year. According to Melanoma New Zealand our melanoma incidence rate is the highest in the world. In New Zealand we are especially vulnerable to skin cancer with our high rates of UV radiation. Anyone can develop skin cancer though it is most common in people with the fairest skin types. Main risk factor for skin cancer – regular unprotected sun exposure.
We recommend regular skin checks and mole surveillance by a professional provider. This regular surveillance provides comparisons year on year. Melanomas are not only moles or spots that change in appearance or grow. A melanoma may also present as a firm, red or nodule-shaped lump or bump.

ABCDE – a rule for spotting melanoma
While the ‘ABCDE’ rule (asymmetry, border, colour, diameter, evolving) is a guideline for spotting unusual spots or moles on your skin, you can also use this rule for any suspicious lumps and bumps, especially ‘evolving’ or growing, even if this is slowly.
Early detection of any lumps and bumps will often mean less invasive treatments are necessary. Get in touch with our specialists, send us a photo if possible, if you have discovered a new lump or bump or if you have an existing lump or bump that has changed or is growing. We can diagnose the cause and recommend a treatment option, which may include removal or simply leaving it.

While not every lump or bump is cancerous, you may want it removed because it is unsightly, annoying or symptomatic causing pain or discomfort. Sometimes, lumps and bumps become infected. They may need to be drained and treated with antibiotics first, with a plan in place for removal (usually under local anaesthetic). Lumps and bumps may catch on your clothing or get irritated because you constantly knock them. Your lump or bump may be somewhere that causes you embarrassment, for example, on your face, forehead or nose.
If you have a suspicious, unsightly or annoying lump or bump, have it checked by our team of experienced specialists and surgeons. An ultrasound scan may be needed to confirm diagnosis. Treatment for lumps and bumps starts at $1,200.
Refs:
The Cancer Society https://www.cancer.org.nz/
Melanoma New Zealand https://melanoma.org.nz/
What is the reason behind Donald Trump's big swollen ankles?
Photo credit: AP, Stuff 18 July 2025
You may have seen in various news media here and overseas that Donald Trump's ankles appear swollen. The diagnosis, according to his personal doctor, is chronic venous insufficiency. Is there cause for concern?
What is Chronic Venous Insufficiency and Swollen Ankles?
Chronic venous insufficiency (CVI) is a condition characterised by failure of the venous valves within the surface and deep veins of the legs. This causes blood to pool in the legs causing varicose veins, leg and ankle swelling and sometimes skin problems, such as ulcers. CVI is a relatively common condition and can deteriorate over time. People with leg swelling should consult with their general practitioner (GP) or vascular specialist for diagnosis and appropriate management.
Some other causes of leg swelling include heart failure and other major medical conditions, lymphoedema, and lipoedema.

What Causes Chronic Venous Insufficiency?
CVI usually results from venous valve failure, which impairs the upward flow of blood from the legs towards the heart. Other risk factors include:
- Prolonged standing or sitting: this causes increased venous pressure over time contributing to valve damage. People who stand at work for long periods or who travel long-distance regularly.
- Deep vein thrombosis (DVT): a dvt is a blood clot in the vein. Blood clots can damage valves.
- Obesity: being overweight can increase pressure on the veins and valves.
- Pregnancy: sometimes hormonal changes, with the corresponding increased blood volume, can stress venous valves.
- Age: valve function diminishes naturally over time.
- Family history of the condition: a family history of CVI can mean the condition is passed on.
What are the symptoms of CVI?
The most common symptom of CVI is leg swelling, especially swollen ankles. Fluid gathers, mostly worse when standing, and improves when legs are elevated. Varicose veins, large ropey-looking veins on the surface, are also associated with CVI. Along with varicose veins, patients often describe a feeling of heaviness in the legs. And their legs also ache. A patient might also notice skin changes on their legs. These may become itchy with eczema and noticeably red or darker and patchy. An ulcer may form if the skin continues to deteriorate, often after minor trauma.
Any leg swelling is uncomfortable; the legs may feel hot, heavy and as if they are 'bursting'.
What treatment do we recommend for CVI?
Following a consultation, advice on risk factor management and a venous ultrasound scan, we will recommend the best treatment path. In the first instance, and for more immediate relief, we will recommend medical-grade compression stockings/socks. These are graduated so help to disperse the fluid and encourage blood flow. All in all, a patient will get some relief from the pressure that has built up to cause the swelling.

If varicose veins are present, we will recommend non-invasive treatment to close off the veins so blood can re-route via healthy veins.
Donald Trump meets many of the risk criteria above: age, long periods sitting, because of his extensive long-distance travel, and swelling in his ankles. Ultrasound scans will confirm a diagnosis of CVI and rule out any other serious conditions, such as DVT.
Refs:
Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2014;130(4):333-346
Nicolaides AN. Investigation of chronic venous insufficiency: A consensus statement. Circulation. 2000;102:E126-E163.
What's the best option for skin tag removal?
We recommend sending us photos by email or completing our online consultation inquiry. Our nurse will talk to you about your best option for skin tag removal.
Please note: skin tag removal must be performed by a skin specialist, general practitioner or surgeon. This is imperative if your skin tag is in or around the delicate area of the eye or eyelid.
The skin tag may look like it could twist off but if you attempt this yourself you may cause bleeding, infection or scarring.
What is a skin tag?
Skin tags are little, benign growths that hang on the skin. They are common and usually soft and flesh-coloured or slightly darker. Mostly they will hang by a thin stalk. They are raised and can look knobbly, with a build up of skin. While skin tags are normally harmless they do have a blood supply connected to your body, so care needs to be taken when having them removed. Most often they will be in areas where skin rubs against itself or clothing and they are easily knocked. Commonly on the neck, underarms, groin or eyelids.

What causes a skin tag?
Skin tags are more likely to develop owing to:
- Age, as they're more common in middle-aged and older people
- Friction from clothing or skin folds
- Hormonal changes, such as during pregnancy
- Being overweight, because skin tags may form in skin folds
- Conditions like diabetes
- Genetics, as they can run in families.
When should you have a skin tag removed?
In most cases, skin tags have no health risks. But you may consider having one removed if it becomes irritated, bleeds or because you are constantly knocking it. Or it catches on clothing or jewellery or you simply don’t like the look of it. If your skin tag is near or on your eyelid, it may be annoying as you feel it when you blink or see it in your peripheral vision.
If your skin tag bleeds or changes in some way, for example, the colour changes, the feel of it changes or it grows, then it is time for it to be removed.
Contact us if you have concerns such as these about your skin tag or if you are not sure that it is in fact a skin tag and want a diagnosis to confirm. Contact us, too, if you just want it removed. Complete our online consultation inquiry and send us photos and our nurse will contact you to discuss the best options for treatment.

How we remove skin tags
Small skin tags can be shaved off with a sharp scalpel blade or frozen off with liquid nitrogen. If the skin tag is larger our surgeon will remove it under a local anaesthetic, where the skin tag and surrounding skin is numbed and then the skin tag is excised. You are awake during the procedure.
Usually, no sutures are needed and just a plaster will cover the small wound.
How long does skin tag removal take?
This is a quick procedure.
Skin tag removal typically takes 10-15 minutes, depending on the size of your skin tag and where it is on your body.
Check out our minor surgery pages for more information.
Can you fly long distance now you've had your veins treated?
This is another of our FAQs: when is it safe to fly long distance after my varicose vein treatment?
There are a number of factors to consider when embarking on long-distance travel after treatment, even by car. Domestically, we say it’s okay to travel straight away as long as you stop and walk around every 30 minutes for five minutes or so. Travelling overseas on a long-haul flight is more problematic.
It depends on what treatment you’ve had, whether you’re prone to blood clots (DVT, deep vein thrombosis) or have other medical conditions that increase your risk eg, being overweight or having reduced mobility. As well as your overall health. Keeping physically fit, not smoking and maintaining a healthy weight.

The reason all this is important is because you need to keep your circulation going and blood pumping back to your heart. Any long-distance travel carries a risk of blood clots, more so if you’ve recently had surgery, including a minimally invasive vein procedure. Cabin pressure and sitting for long periods may also cause your legs to swell.
Let us know your plans before your procedure so we can advise on when it’s safe to travel. We are also happy to see you after your trip for peace of mind.

We recommend waiting before travelling long distance
Usually we recommend waiting at least four to six weeks before flying long haul. Four weeks for Asia/US and six weeks for Europe. If you’ve had:
- Minor sclerotherapy: patients can fly short distances within three to seven days but for long-distance flights we recommend waiting two to four weeks to reduce the risk of blood clots.
- Minimally invasive varicose vein treatment: wait at least four to six weeks as above. Because the veins need time to heal and potential clot risks needs to be minimised.
- Below-knee compression stockings/socks should be worn with all air and road travel.
It’s been 4-6 weeks can I fly long distance now?
Even after waiting four to six weeks, we recommend the following during your flight:
- Wearing medical-grade compression stockings to promote blood flow and reduce the risk of swelling or clots.
- Moving around the cabin during the flight and doing seat exercises to help with circulation.
- Drinking water and avoiding alcohol; as alcohol dehydrates this can inhibit circulation.

If you have had a DVT before, talk to our vascular surgeon. He may recommend taking blood thinning medication.
Is the strange sore on my leg a venous ulcer?
A venous ulcer – caused by underlying varicose veins.
This ulcer is an open wound or sore that takes a long time to heal, comes back again or doesn't heal at all. Leg ulcers have various causes, including varicose veins, blocked arteries and swollen legs from excess fluid around the ankles. Diabetes may make this condition worse. If you think you have a leg ulcer it is important to consult a vascular specialist.
What is a venous ulcer?
Venous ulcers occur due to poor blood circulation in the veins, causing increased pressure on the skin. They occur on the lower legs. The leg may be swollen and there may be other skin changes, such as eczema, itching and discolouration.
Venous ulcers are often not particularly painful, unless they are infected.
What does a venous ulcer look like?
A venous ulcer is an open wound with:
- An irregular shape
- Shallow depth
- A red base, sometimes covered with yellow tissue
- Swollen, discoloured or hardened skin
- Surrounding skin that looks dry and scaly
- Itchy skin.

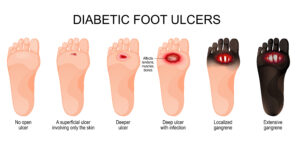
Other ulcers include: arterial ulcers and diabetic ulcers
Arterial ulcers – caused by poor blood flow through the arteries. Will most often be found on the feet, heels or toes and are often painful, especially when they are infected.
Foot ulcers are more likely in people with diabetes. A diabetic ulcer is often difficult to heal because of underlying blood circulation issues, a complication of diabetes. If you have diabetes and a suspected foot ulcer, it is important to seek treatment early. See below for how a diabetic ulcer can progress without treatment or attention.
What does the path to treatment for a venous ulcer look like?
Because ulcers are distinctive open sores that don’t heal easily, you will most likely see your general practitioner (GP), community nurse, nurse specialist or nurse practitioner first. They will refer you to a vascular specialist but you can also refer yourself. The most important thing is to get on to treatment early.
Our vascular specialist will recommend treatment options, including prescribing antibiotics if there is an infection and an ultrasound scan to test the arteries and veins. Next, they will often refer you to our nurse clinics for wound dressing and maintenance.
Our experienced nurses take care of your venous ulcer
We assess, treat and offer advice for ulcers in our specialist nurse clinics. We clean and dress the ulcer in a sterile environment. Our nurses are available to answer questions about your ulcer and follow up to check on your progress. We will refer you back to your GP practice or to the community nurses once the ulcer is healing.

Wearing compression socks maybe recommended
Wearing compression socks often helps improve blood flow and can reduce swelling. This aids the healing process for an ulcer. Best worn when healed or nearly healed.
In some cases, surgery may be necessary to improve blood flow or remove dead tissue from an ulcer. Skin grafts may be an option for large ulcers or those that don’t respond to other treatments.
What can you do to help healing and prevent an ulcer recurring?
While regular exercise may be difficult at first, adopting a healthier lifestyle can improve the healing process. This includes gentle exercise, you might do seated or floor exercises at first and progress to walking. Eating a balanced diet and following instructions on living with conditions like diabetes also help ulcers to heal.
It is important to seek advice early whenever you suspect you have an ulcer. And once your ulcer has healed we recommend regular check ups.
Helpful information on how much time varicose vein treatment takes
In response to the most frequently asked question when patients call us, we break down the time varicose vein treatment takes. We say on the day of your treatment allow an hour an a half, as that will be enough time for the consent process, treatment and recovery.
You need an ultrasound scan before treatment
Before varicose vein treatment, we ask patients to have an ultrasound scan. We will arrange an ultrasound scan for you. This means when you see the vascular specialist they are armed with a map of your veins and can advise on treatment immediately. An ultrasound scan usually takes between 30 and 60 minutes, depending on whether you need one or two legs treated, how severe your varicose veins are or if your varicose veins are in another part of the body, for example, the pelvis.
How much time does the ultrasound scan take? It takes: 30-60 minutes.

Next is your consultation with the vascular specialist or vascular specialist nurse
This appointment will typically be for about 10-15 minutes. Many patients prefer to talk with the vascular specialist or vascular nurse specialist over the phone. You will need to provide them with photos of your varicose veins for this. The phone consultation takes the same amount of time as an in-person consultation.
You can complete our online form, too. The vascular specialist or vascular specialist nurse will evaluate the condition of your varicose veins and discuss treatment options, if necessary.
How much time does the consultation take? It takes: 10-15 minutes.
Treatment day: your consent and pre-procedure information
Our nurse will call you a couple of days before treatment. On the day, the nurse will prepare you for your treatment, check your personal details and give you a gown to put on. Next, the vascular specialist will explain the procedure again, answer any questions, talk about the risks and benefits of treatment and get your signed consent to go ahead.
How much time does the consent take? It takes: 15 minutes.

How much time varicose vein treatment takes
How much time varicose vein treatment takes depends on the type of treatment:
VenaSeal medical adhesive
This procedure involves sending droplets of medical glue down a catheter inserted into the vein to seal off the vein so it will eventually fade. We predominantly use VenaSeal for our varicose vein treatments.
How much time does time does the VenaSeal procedure take? It takes = 15 minutes per leg (other areas of the body take longer).
Endovenous Laser Treatment (EVLT) or Radiofrequency Ablation (RFA)
EVLT/RFA typically takes about 45 to 60 minutes. This minimally invasive procedure involves inserting a laser fibre into the vein to seal it shut.
How much time does time does EVLT/RFA treatment take? It takes: 45-60 minutes.
Sclerotherapy
Sclerotherapy involves injecting a solution (sclerosant) into the smaller varicose veins to make them to close. This precise treatment is most often performed immediately after VenaSeal treatment. It usually takes about 20-30 minutes.
How much time does sclerotherapy treatment take? It takes: 20-30 minutes, depending on how many smaller varicose veins need treating.
When can you leave to go home after varicose vein treatment?
After the procedure, you will be fitted with thigh-high compression stockings, then patients are monitored for about 20 minutes but can walk out of the treatment room. It is okay to go home after 20 minutes. We recommend someone drive you home.
How much time does observation take? It takes: 20 minutes.
How long is the at-home recovery time for varicose vein treatment?
Because the treatment is minimally invasive patients can resume normal activities within a couple of days. Our nurse will call you a day or so after treatment to check on you. Patients may experience some bruising, swelling and discomfort, which typically improves within a few days to a week.
How much time does at-home recovery take? It takes: 2-3 days.
How long is the follow-up appointment for varicose vein treatment?
Most often our nurse will check in on you again at the six-week mark. An appointment to call you will be made before you leave the clinic. If you have any concerns before this, please call our nurses. You can also ask for the vascular specialist to contact you for a follow-up appointment. These appointments are very quick so we recommend a phone call follow up.
How much time does the follow-up appointment take? It takes: 5-10 minutes.
Recovery, including the resolution of swelling and bruising, can take several weeks to months.
Note: these are based the times it usually takes. This may vary between patients.
We offer better options than vein stripping of varicose veins
The main reason we don't strip varicose veins any more is because there are now far less invasive treatments available. But it's still a myth that varicose veins are stripped out. It is often the main reason why people leave varicose veins untreated.
We use a minimally invasive form of medical adhesive to seal off the vein called Venaseal. It starts with a local anaesthetic so the patient is awake throughout. Tiny amounts of the adhesive are deposited along the vein. The adhesive works by reacting with your own blood, making it sticky enough to seal the vein – it is your own blood that is actually doing the sealing. Both the sealant and the vein will gradually be absorbed by the body over time.
By using this method it means the patient can resume normal activities much faster compared to vein stripping. Vein stripping is an operation with many weeks recuperation. Among the benefits of these modern treatments, which have been in New Zealand for many years, are fewer complications from treatment and less pain during. Plus long term, the outcomes are better, the veins are more likely to fade more quickly and cosmetically the patients veins will look better.
Sclerotherapy, where a sealant is injected into smaller veins, is another modern method used by the vein specialist. This is usually done at the same time as the 'medical glue' procedure. As with 'medical glue' (Venaseal) this treatment method is less invasive with better outcomes than when veins were stripped.

Can you leave varicose veins untreated?
Varicose veins are a medical condition and, contrary to belief, not just a cosmetic one. As with any injury or condition the more quickly the issue is dealt with, generally the better the outcome for the patient. When veins become varicose it means they are no longer doing their job of transporting blood back to the heart. The blood is pooling and sluggish. While symptoms, like heavy legs and aching legs, may be experienced, it is the bulging, ropey look of varicose veins that highlight the issue for most patients. Leaving varicose veins untreated is generally not recommended, as they can lead to several complications, see below.
When to worry about varicose veins
While some individuals may not experience any significant symptoms initially, untreated varicose veins can cause discomfort, swelling and pain over time. More severe complications may include skin changes, ulcers, blood clots and bleeding. It's important to seek medical advice to manage varicose veins effectively and to help prevent these potential issues.
You can start by wearing compression stockings to help relieve symptoms, especially if you stand all day. Compression stockings help keep blood circulating. But these generally provide short-term relief. The best option is to have a consultation at a vein clinic with a vascular specialist who will organise an ultrasound scan before your appointment to diagnose the severity of the issue.

Is sclerotherapy the best option for your veins?
What is sclerotherapy and how is it used?
Sclerotherapy is a medical procedure used to treat varicose veins. A solution of vein irritant is injected directly into the affected veins using ultrasound guidance. This causes them to collapse forcing blood to re-route through healthier veins. The collapsed veins are reabsorbed into the body and eventually fade. Sclerotherapy is a precise, minimally invasive process. It's known for being effective and having a quick recovery time. We usually offer sclerotherapy either as your main varicose vein treatment or in combination with closing down the main feeding vein. Sometimes, after varicose vein treatment, you will need some sclerotherapy to tidy up any remaining small varicose veins.
When is sclerotherapy used instead of other vein treatments?
Sclerotherapy is a common component of most varicose vein treatments. Some patients will only need sclerotherapy for their vein treatment but many patients will also need treatment for a leaking surface vein. This treatment will usually involve a sealant treatment (Venaseal) or a heat treatment such as laser/radiofrequency. All of these vein treatments have been shown to be equally effective and safe. Almost all procedures take about 30-60 minutes, are minimally invasive and the patient is awake throughout.

Microsclerotherapy is also used for spider veins and very small varicose veins. When the remaining spider veins are too small to be treated with microsclerotherapy, we recommend laser therapy for treatment. Laser therapy uses focused light to heat and damage the veins, causing them to slowly disappear.
A combination of both treatments may be recommended to achieve the best results.
How do you know if you have varicose veins?
Usually varicose veins are visible and patients already know what they are from their appearance and their symptoms. To find out the cause of varicose veins, an ultrasound scan guides the vascular specialist to where the varicose veins are being fed from. Sometimes clusters of spider veins are an indication that underlying varicose veins are the cause. An ultrasound scan scan will determine if this is the case.

Consulting with a vascular surgeon is essential to determine the best treatment plan and the best method of treatment if you have varicose veins.